by iphindia | Feb 15, 2017 | Blog
India and the world in 2016: a challenging present, an uncertain future
Google’s “See what the world searched for in 2016” says it all: how has the year 2016 been so far for all of us? Four out of five of the top most trending global news searches relate to disasters – until we started talking about the Rio Olympics. I like the quote there, though, “love is out there”, and on a personal note I’d like to add, “Where hope is lost” and if not lost, speedily fading away.
My country is not alien to this context and process. Of late, when the whole world just focused on a single election and individual, predicting “not so happy” consequences and a whole lot of uncertainties, we Indians were not so startled. Yes, being a stable yet very peculiar economy in our region, sensitive to foreign investment, the Indian rupee, market equities, and trade did slide for a moment following the incredible (unexpected) US electoral results. However, we were not as surprised as many others, perhaps because we had other things to be surprised at. ……(Coincidentally the US election results and the demonetization announcement in India happened on the same day)…… I guess, collectively we are now adjusted to ‘uncertainties’- although with positive hopes.
However, we were not as surprised as many others, perhaps because we had other things to be surprised at. ……(Coincidentally the US election results and the demonetization announcement in India happened on the same day)…… I guess, collectively we are now adjusted to ‘uncertainties’- although with positive hopes.

by iphindia | Feb 15, 2017 | Blog
The ev4gh is an innovative multi-partner blended training program for young, promising and emerging health policy & systems researchers, decision makers and other health system professionals.
This program gives an ideal platform for these young minds to voice their views and understanding on global health issues while being rooted in their local/regional realities. The program entails a distance coaching phase followed by a face to face training phase, the later being usually organised preceding the global symposium on health systems research bi-annually.
Manoj was fortunate to be part of this program as an EV 2016. Additionally being the official correspondent for the symposium this time,he took the opportunity to interview the man who started this innovative training program six years back- founding father of ev4gh initiative- Prof Wim Van Damme from the Institute of Tropical Medicine, Belgium.
Here is the to watch that interview
link!
For those want to know further on ev4gh,
here is the website.

by iphindia | Nov 22, 2016 | Latest Updates, Blog

Manoj Kumar Pati is a public health researcher at the Institute of Public Health, Bengaluru. He has a masters in public health (MPH) in health system management. His research interests are implementation research, equity research, epidemiology and non-communicable diseases.
We are increasingly seeing several service delivery programmes running at country level, particularly in South East Asia. For example, in India, we have seen the implementation of many programmes that are top-down and vertical in nature. Citizen demand has never been considered while implementing social security schemes for health and different political environments present significant challenges for sustainable service delivery.
 We heard the voices of young health systems researchers and their mentors loud and clear the Emerging Voices for Global Health (EV4GH) organized session on day one of the Fourth Global Symposium on Health Systems Research. The EV4GH, is a unique Thematic Working Group of the Health Systems Global.
We heard the voices of young health systems researchers and their mentors loud and clear the Emerging Voices for Global Health (EV4GH) organized session on day one of the Fourth Global Symposium on Health Systems Research. The EV4GH, is a unique Thematic Working Group of the Health Systems Global.
The opening plenary of the Symposium, set the scene for the challenges faced by the global health community highlighting the need for resilient and responsive health systems in the 21st century. The diverse panel brought a range of issues to the table from citizen’s choices and voices, primary health care, universal health coverage (UHC) to issues of health of immigrants and migrants.

by iphindia | Nov 21, 2016 | IRP, Blog, Latest Updates

The Soliga people of southern India continue to live within and around forest areas. Their history, tradition, and culture are deeply rooted within the forests in which they live. In an increasingly globalised world, their ways and means slowly erode as they inch towards the unfulfilled promises of development.
To read more: Click here

by iphindia | Apr 21, 2016 | Blog, Latest Updates
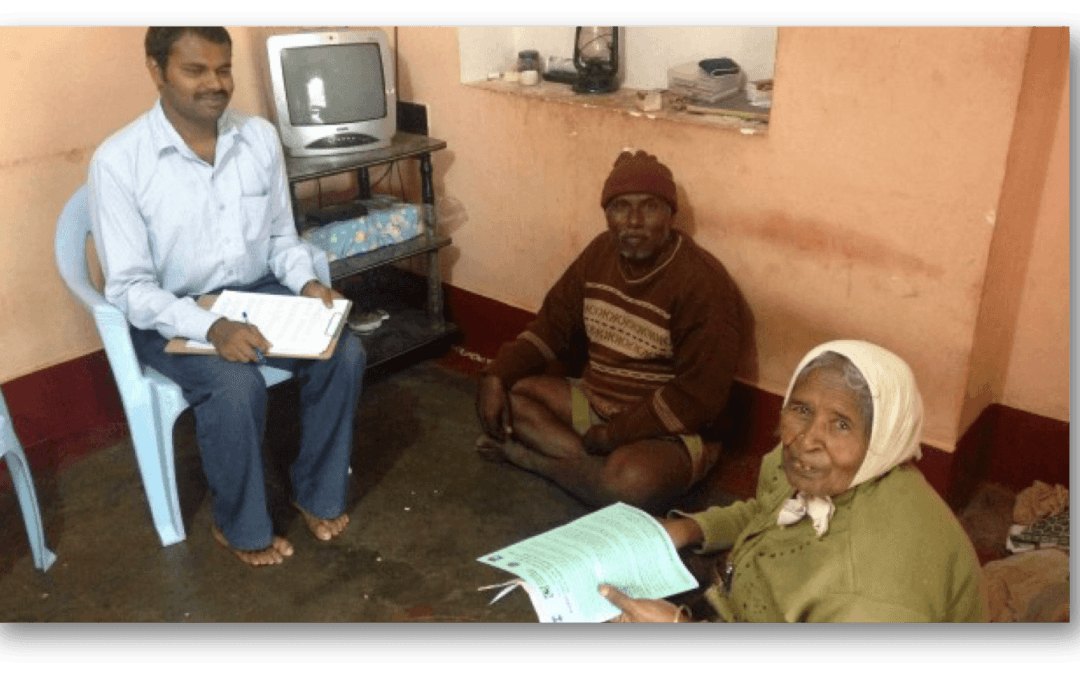
 The art of data collection in health system research: Lessons learned from the field.
The art of data collection in health system research: Lessons learned from the field.
Data collection is the most important aspect any research endeavour. Poor quality of the data will have impact on the results of the research study.Therefore it is vital for the researchers to adopt appropriate data collection methods to ensure quality data.Here is a blog by Meena Putturaj which highlights the practicalities of data collection in health systems research based on the field experiences.
Data collection is a crucial aspect of any research project. Depending on the nature and scope of the research question, collecting quality data requires considerable investment of time and resources. Indeed, any research endeavour is handicapped without the relevant data.
During a recent health systems research project, I had to collect a lot of information from government agencies, which turned out to be no cake walk. There were occasions when I had to wait for hours at a time to collect documents, to meet officials, and to conduct interviews. Those waiting periods gave me sufficient time to observe and reflect on the functioning of some of the government agencies in India.
Health systems research often requires data from, and cooperation by, the state sector authorities. So, as a rule of thumb, the health systems researchers work closely with government officials and will require data from them, the interpretation of which might reflect negatively upon those state sector authorities. This can, I think, make some officials and other employees feel that they are being cross examined or interrogated when researchers go to collect data from them. The various situations that I’ve been in while collecting data from government officials have enabled me to develop skills to deal with this tension and the struggle of getting relevant data. The following strategies have worked well for me while trying to obtain data:
To read more about “The art of data collection in health system research” : Click here

by iphindia | Mar 16, 2016 | Blog, ATM, Latest Updates

Dr Praveenkumar Aivalli blog titled, ” What I learnt from my first health system research project ” published in BioMed Central
Starting my first research project
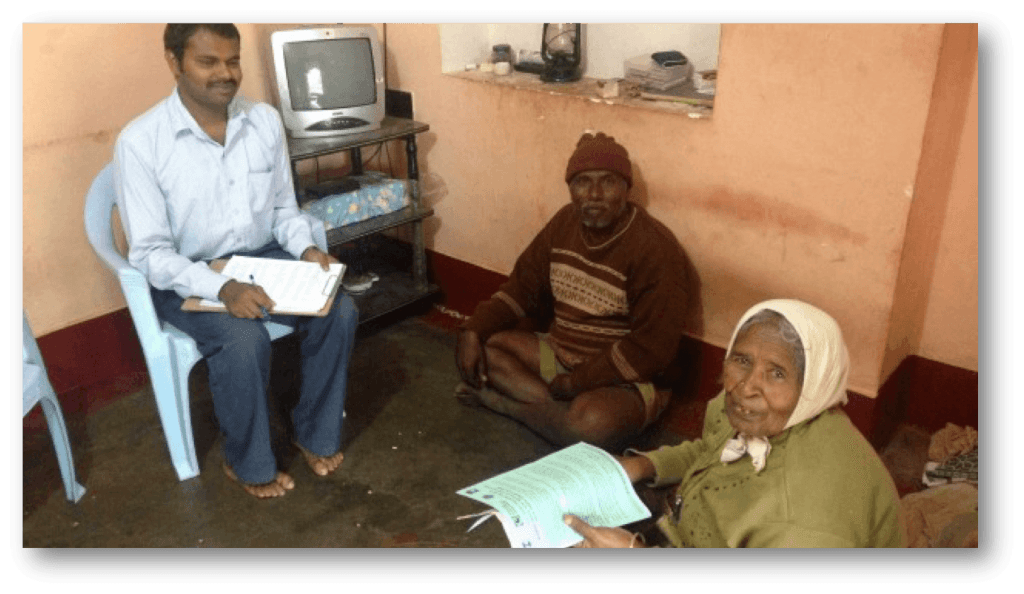
Back in 2013, I just stepped out of my university after getting my Master of Public Health degree, in no time I was given an excellent opportunity to work on a World Health Organization (WHO) funded health system research project in one of the reputed public health research institutes in Bangalore. It was the first research project of my public health career and as a new bee, I was buzzing with excitement and enthusiasm about the study.
The project was on improving NCD (Non Communicable Diseases) care at primary health centers in one of the districts in south India. It was a quasi experimental study trying to understand the impact of health system interventions through a baseline and end line household and facility surveys.
For better coordination, exposure and learning, I was placed in the study district. Having completed most of my education in the country, it was not that difficult for me to understand our country’s health system.
We visited more than 1000 families to get data on NCD care at the rural level, health seeking behaviors of NCD patients and their out pocket expenditures for NCD care.
The theoretical explanations from classrooms started fitting in its notches when I got exposed to the field during the early days of the project. I got the hang of the project fairly quickly and began preparing for the baseline survey in the year of 2013.
We visited more than 1000 families to get data on NCD care at the rural level, health seeking behaviors of NCD patients and their out pocket expenditures for NCD care. We also visited primary health centers and private pharmacies in the area to collect information on medicine availability.
To read more about Dr Praveenkumar Aivalli blog Click here

 However, we were not as surprised as many others, perhaps because we had other things to be surprised at. ……(Coincidentally the US election results and the demonetization announcement in India happened on the same day)…… I guess, collectively we are now adjusted to ‘uncertainties’- although with positive hopes.
However, we were not as surprised as many others, perhaps because we had other things to be surprised at. ……(Coincidentally the US election results and the demonetization announcement in India happened on the same day)…… I guess, collectively we are now adjusted to ‘uncertainties’- although with positive hopes.



 We heard the voices of young health systems researchers and their mentors loud and clear the
We heard the voices of young health systems researchers and their mentors loud and clear the

 The art of data collection in health system research: Lessons learned from the field.
The art of data collection in health system research: Lessons learned from the field.